Automated intake and smart routing
Real-time availability and self-service
Preference-based matching and updates
Automated tasks and streamlined workflows
Dashboards and EMR integration
A leading US behavioral health organization faced mounting referral management challenges — fragmented data across EMRs, manual provider assignments, and slow bid processes that delayed care initiation. Provider onboarding was cumbersome, transparency was limited, and administrators lacked a unified view to manage high-volume payor referrals efficiently.
We designed and implemented a Salesforce Health Cloud–powered Referral Management System, integrated with Experience Cloud provider portals, to centralize referral intake, automate provider matching, and enable real-time bid tracking. The solution supported A major American behavioral health institution-driven, provider-driven, and hybrid referral approaches, streamlining onboarding, credentialing, and provider availability updates while maintaining bidirectional EMR integration.
Within weeks of go-live, the organization achieved faster referral assignments, improved provider accountability, and higher participant satisfaction — creating a scalable foundation for efficient payor-provider collaboration and data-driven care coordination.
A leading US behavioral health services organization plays a critical role in supporting payor networks by delivering specialized therapy and behavioral health programs through an extensive provider network.
Handling high-volume payor-referred participants, the organization relies on a mix of internal staff and contracted external providers. Efficient referral management is mission-critical to ensure timely care initiation, adherence to payor SLAs, and improved participant outcomes, while maintaining provider accountability and operational transparency.
The organization’s referral management operations were constrained by structural inefficiencies and fragmented workflows that directly affected participant care delivery and provider accountability.
Referral data from payors, EMRs, and direct engagements lacked a unified system, making it difficult to maintain a single source of truth or track participant journeys end-to-end.
Onboarding and credentialing of external providers were manual and inconsistent, delaying the addition of new providers and resulting in limited real-time visibility into provider availability, service preferences, and compliance with SLAs.
Participant-to-provider assignments relied heavily on manual decision-making or basic rules, leading to inaccurate matching, unfair allocation perceptions, and slower care initiation.
Providers lacked a structured, criteria-based bidding mechanism. Availability, participant preferences, and service compatibility were not dynamically updated, causing delays in bid evaluations and assignments.
Participant demographics, service history, and feedback were spread across multiple systems, preventing a true 360-degree view. This limited administrators’ ability to personalize assignments or reassign based on real-time service performance.
Providers, administrators, and participants operated in silos. Missed updates and delayed feedback loops often resulted in service-level violations, negatively impacting participant satisfaction and payor relationships.
With 90% of referrals coming from a major payor, high-volume participant inflow, and strict SLA commitments exposed operational gaps and made manual processes unsustainable for scale.
With 90% of referrals coming from a major payor, high-volume participant inflow, and strict SLA commitments exposed operational gaps and made manual processes unsustainable for scale.
A referral arrives, and within seconds, the right providers—credentialed, available, and best suited for the participant’s needs—are intelligently suggested. Providers update availability in real-time, participants track progress effortlessly, and administrators focus on outcomes rather than chasing paperwork.
This isn’t wishful thinking. It’s what we at GetOnCRM helped design and deliver—partnering, not just implementing—to transform referral management into a seamless, participant-first experience.
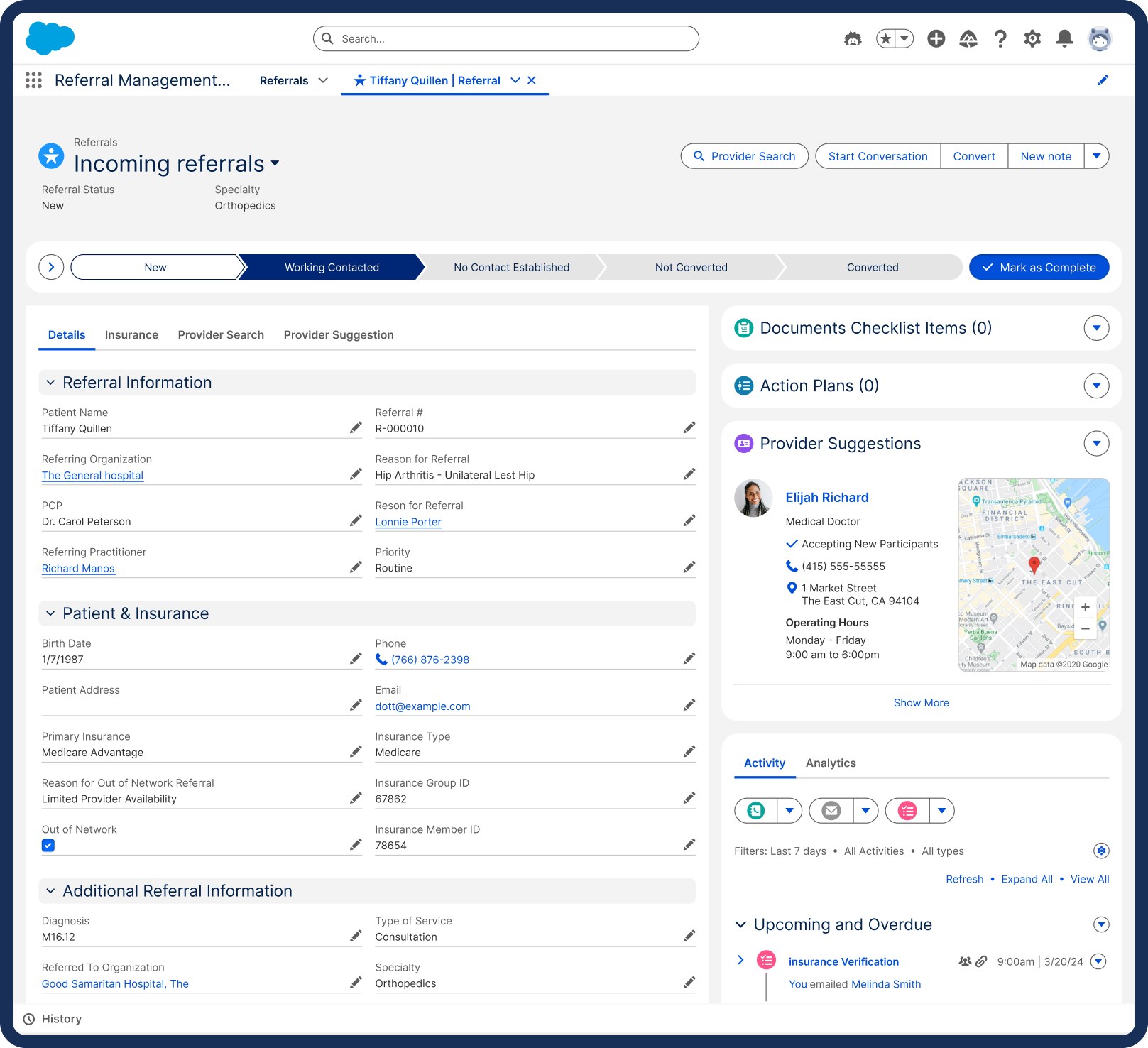
We architected the entire referral journey—intake, qualification, provider matching, bidding, and tracking—inside Salesforce Health Cloud, ensuring every stakeholder works off a single source of truth.
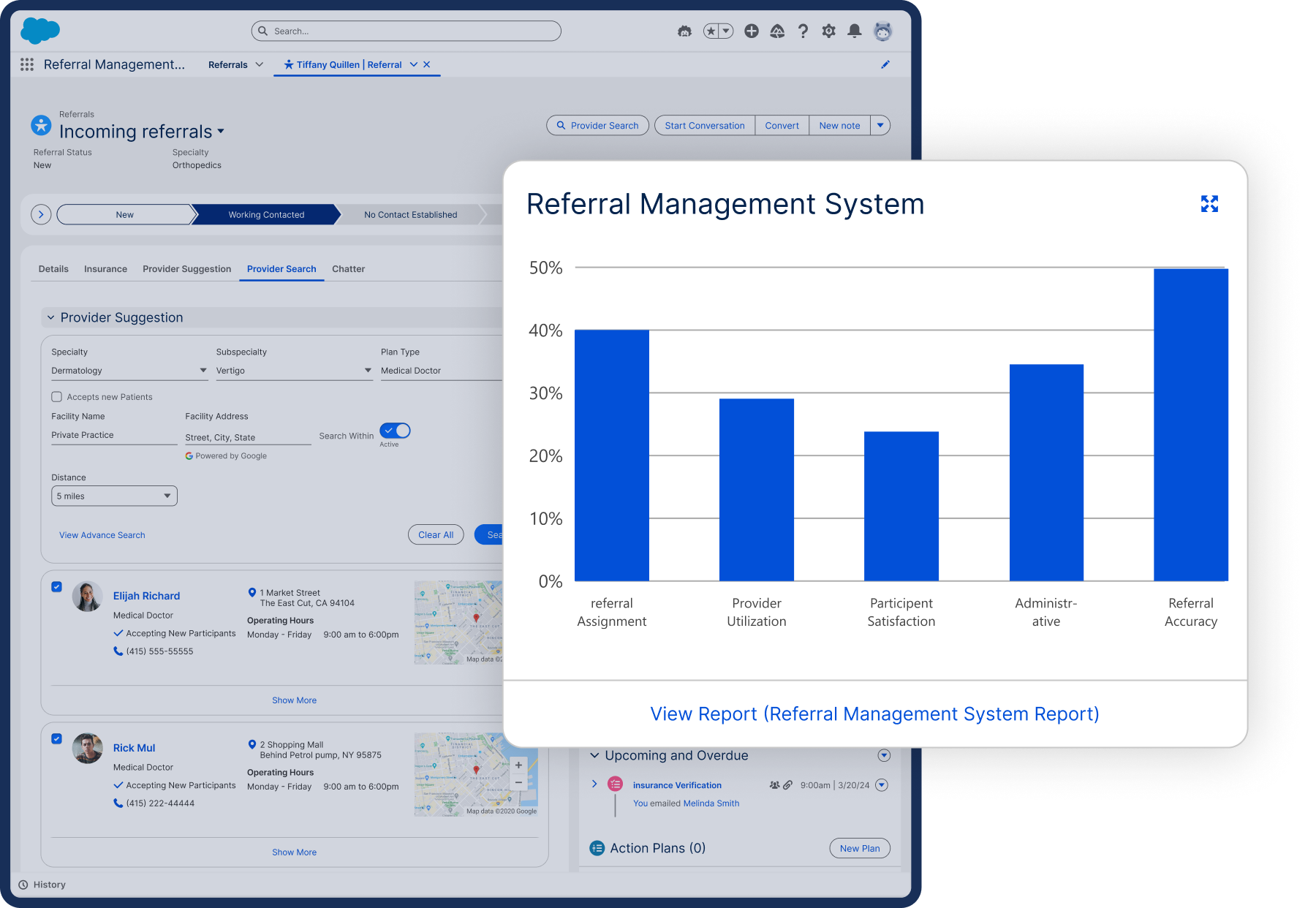
Our consulting team designed a rule-driven engine to move beyond basic filters. Provider credentials, specialties, and live availability now power smart suggestions, supporting hybrid referral approaches without adding operational burden.
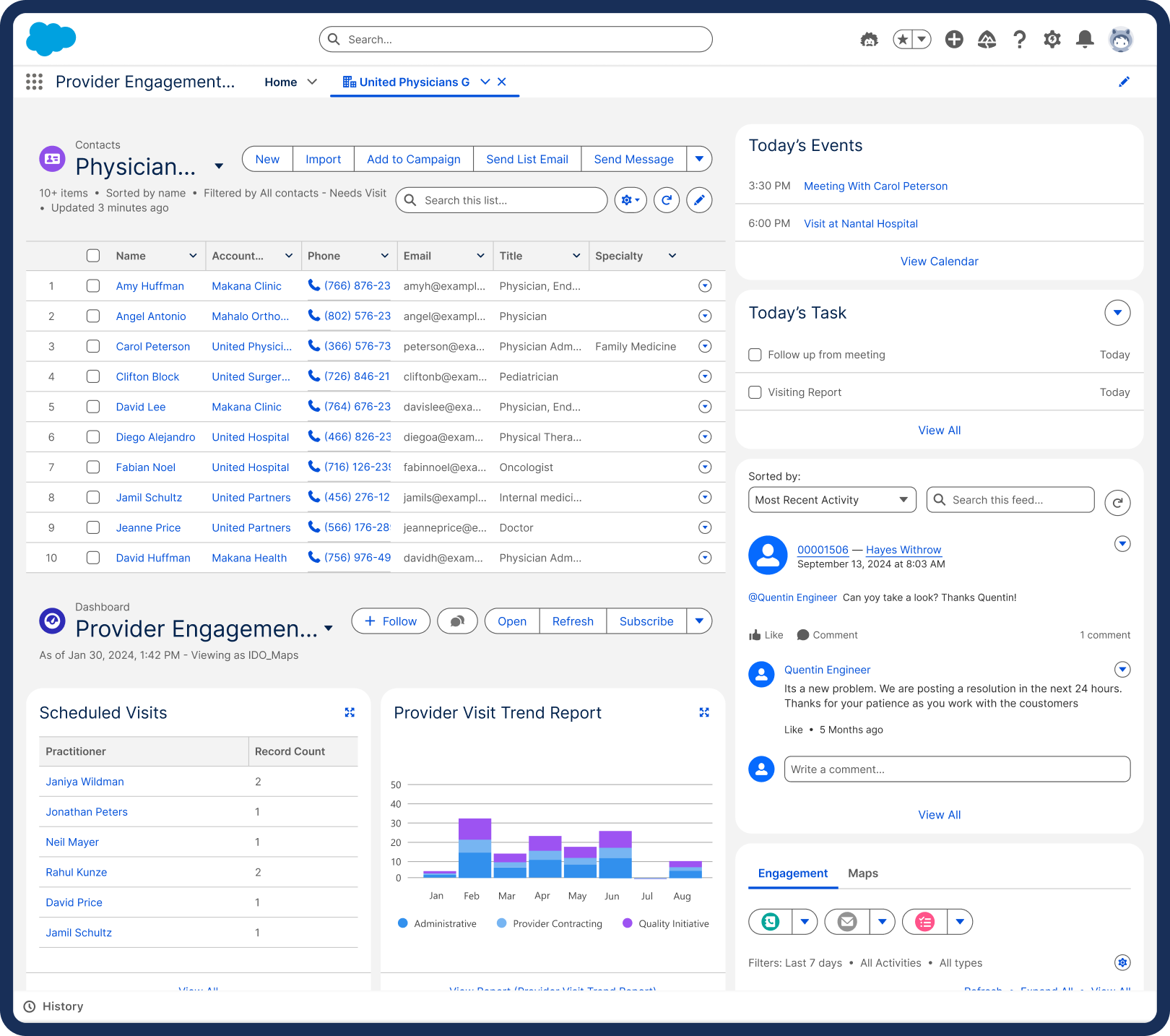
Through the Experience Cloud Provider Portal, we enabled providers to manage profiles, update availability, and bid for referrals effortlessly—turning the provider network into a self-optimizing ecosystem.
The system was designed with a participant-first lens—transparent updates, intuitive provider options, and personalized engagement ensure the process feels less like administration and more like care.
We configured custom dashboards and analytics to deliver actionable intelligence. Network optimization, staffing decisions, and performance improvements are now data-backed and real-time.
Our solution integrates seamlessly with EMR systems, automates workflows to reduce manual delays, and ensures strict role-based security—delivering reliability and compliance from day one.
At GetOnCRM, we approached this not as a vendor delivering a platform but as a strategic partner shaping outcomes. Every design choice was driven by consulting insight, balancing immediate operational wins with a scalable, future-ready architecture.
The result? A referral process that feels almost invisible—fast, intelligent, and participant-focused—transforming referral management from an operational challenge into a strategic advantage.
The Salesforce-powered Referral Management System has delivered measurable improvements across referral operations and network performance:










We are Salesforce Ridge Consulting Partner having 100% salesforce certified team.








Copyright © 2026 GetOnCRM Solutions PVT. LTD. All Rights Reserved.