A leading oncology care provider was managing thousands of prior authorization (PA) requests every day for chemotherapy and diagnostic procedures. The process relied heavily on spreadsheets, manual follow-ups, and fragmented communication among teams.
Operating under both fee-for-service and capitated insurance models, their staff struggled to keep up with growing authorization volumes. Supervisors lacked visibility into workloads, finance teams joined too late for co-pay discussions, and schedulers faced frequent appointment delays.
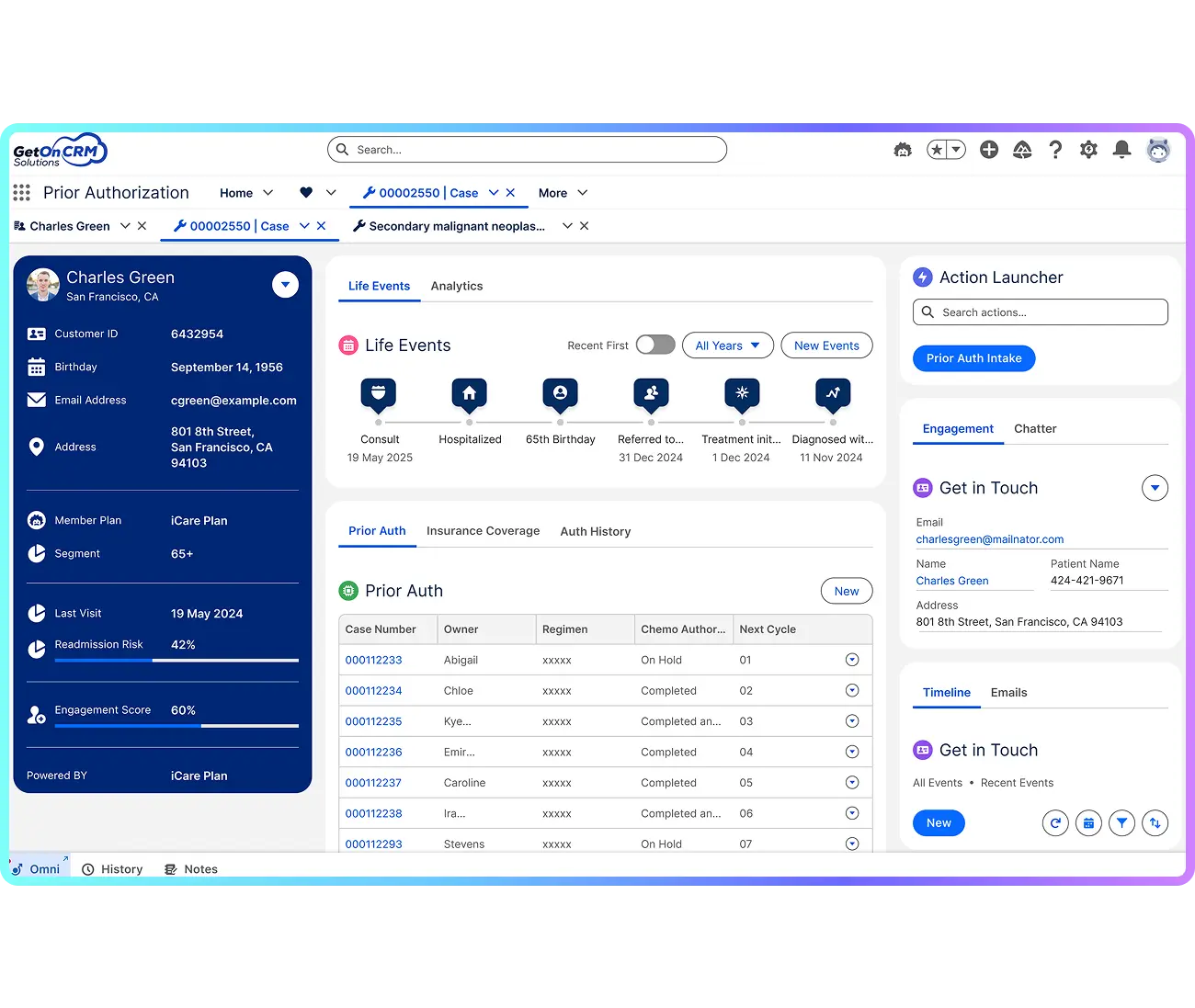
To fix this, the organization partnered with GetOnCRM, a Salesforce Health Cloud implementation partner, to modernize its Healthcare Prior Authorization workflow. The goal was to build a unified, automated, and compliant solution that could improve turnaround time, accuracy, and patient experience.
Goal
Digitally transform the oncology prior authorization process to enhance speed, compliance, and operational visibility.
The client faced multiple workflow inefficiencies that slowed down the authorization process and delayed patient care
Operational Silos
Each team—submitters, coordinators, finance, and schedulers—handled its own tasks with little system-enforced accountability, creating bottlenecks and missed handoffs.
Manual Spreadsheet Tracking
Supervisors manually triaged thousands of orders using Excel sheets. Without real-time updates, it was nearly impossible to identify backlogs or overdue authorizations.
Complex Payer and Insurance Rules
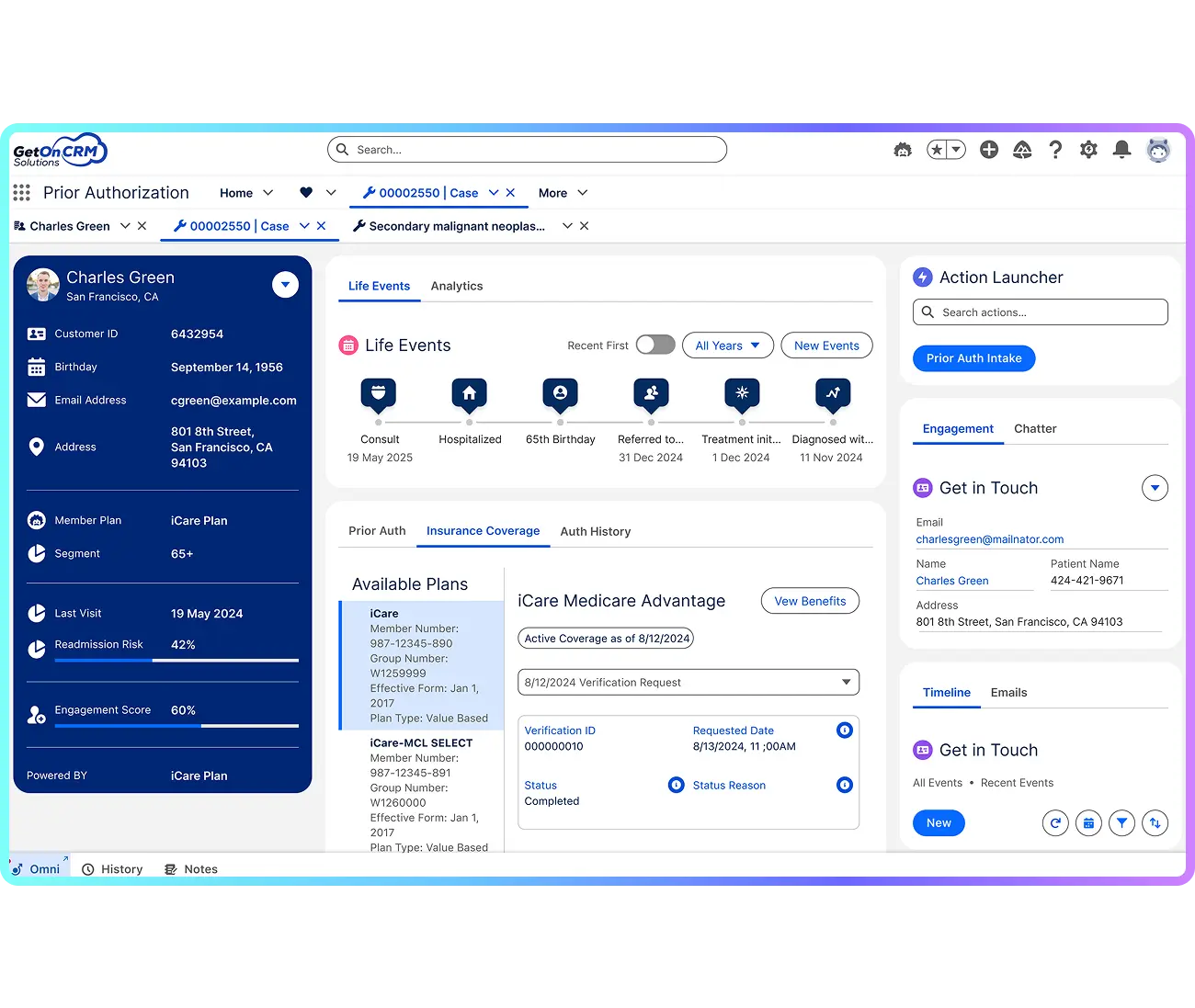
Staff had to interpret payer requirements manually for fee-for-service and capitation models, resulting in inconsistent routing and authorization errors.
Late Financial and Scheduling Alignment
Finance and scheduling teams entered the process late, delaying co-pay verification and appointment booking.
Lack of Scalable Infrastructure
The EMR system lacked automation and audit capabilities, limiting scalability and compliance as the organization expanded its footprint.
GetOnCRM implemented a Salesforce Health Cloud Provider Module that unified all prior authorization operations into one secure, automated platform.
Automated Claim Intake
Claim documents uploaded on the customer portal are automatically fetched into Salesforce. AWS converts PDFs into text for easy AI processing, eliminating manual data entry and reducing turnaround time.
AI-Powered Claim Analysis
The AI engine reviews extracted text, identifies key information, and generates concise summaries with decision-ready insights — helping claim reps validate requests faster and more accurately.
Scalable Data Management
For large or complex claim files, the system vectorizes data using OpenAI embeddings and stores it in Pinecone for quick search and retrieval, ensuring performance at scale.
Salesforce-Centric Automation
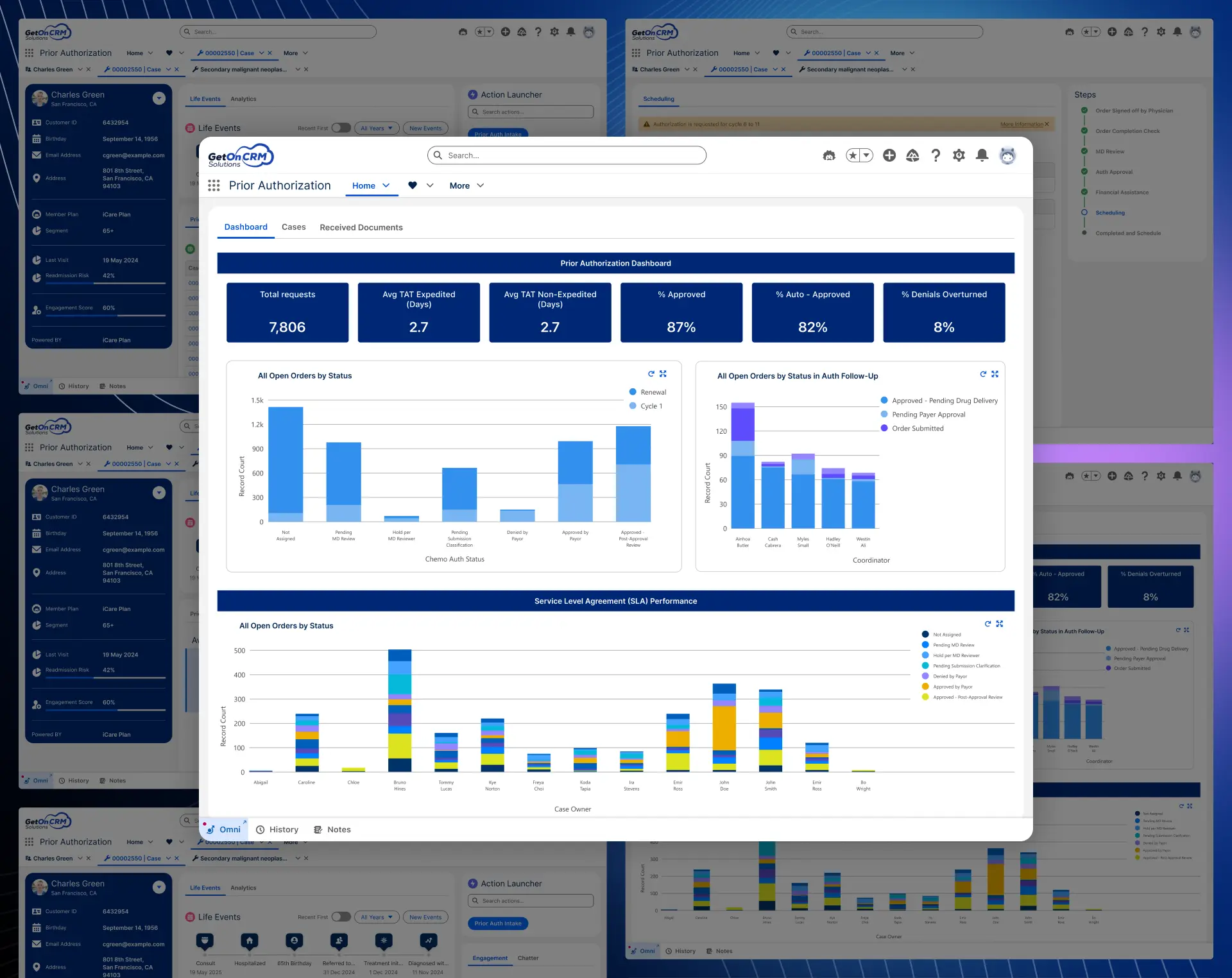
All claim insights are stored in Salesforce, giving teams a unified, automated workspace for validation, approvals, and reporting within a single system.
Oversight, Audit, and Compliance
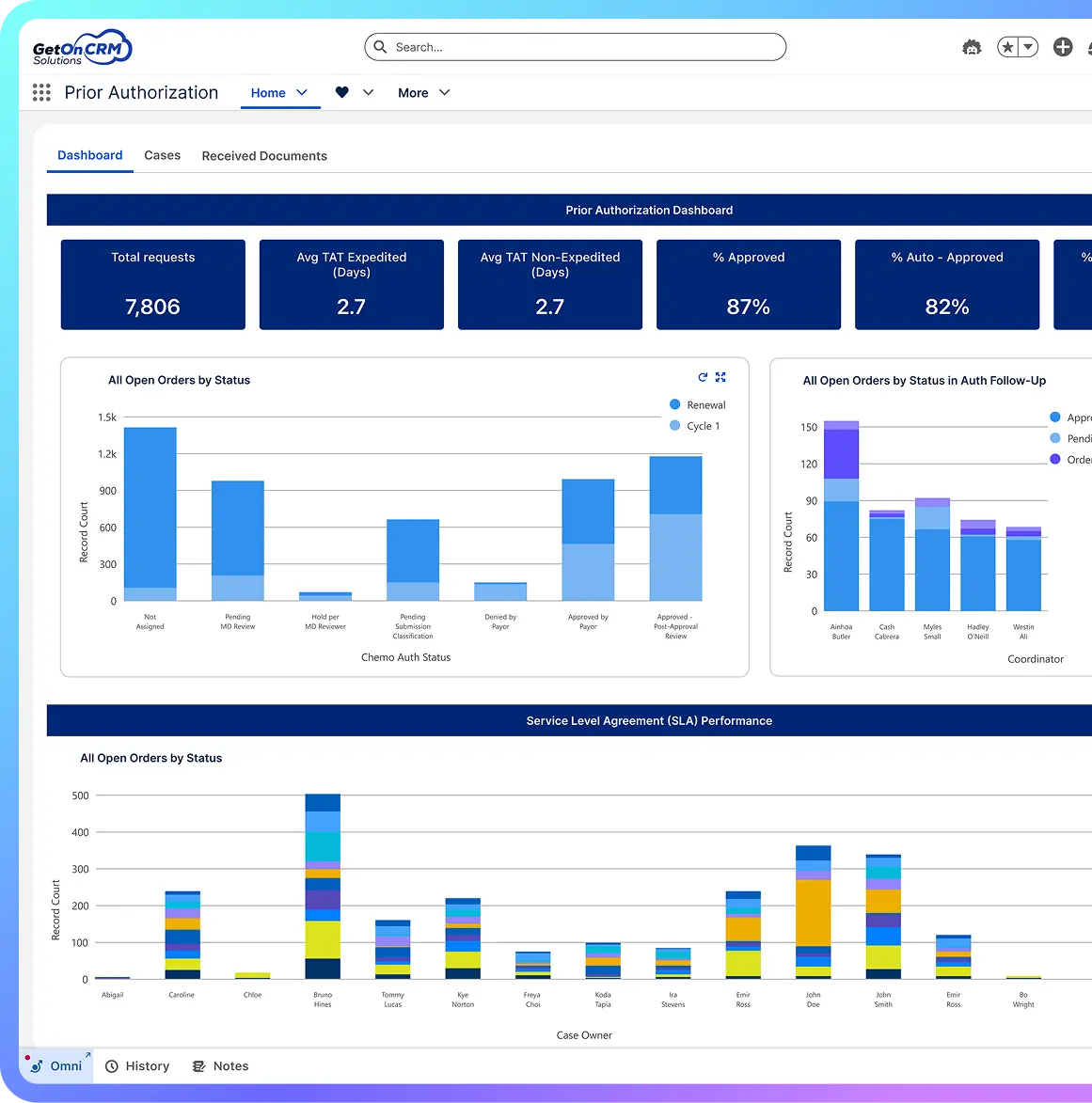
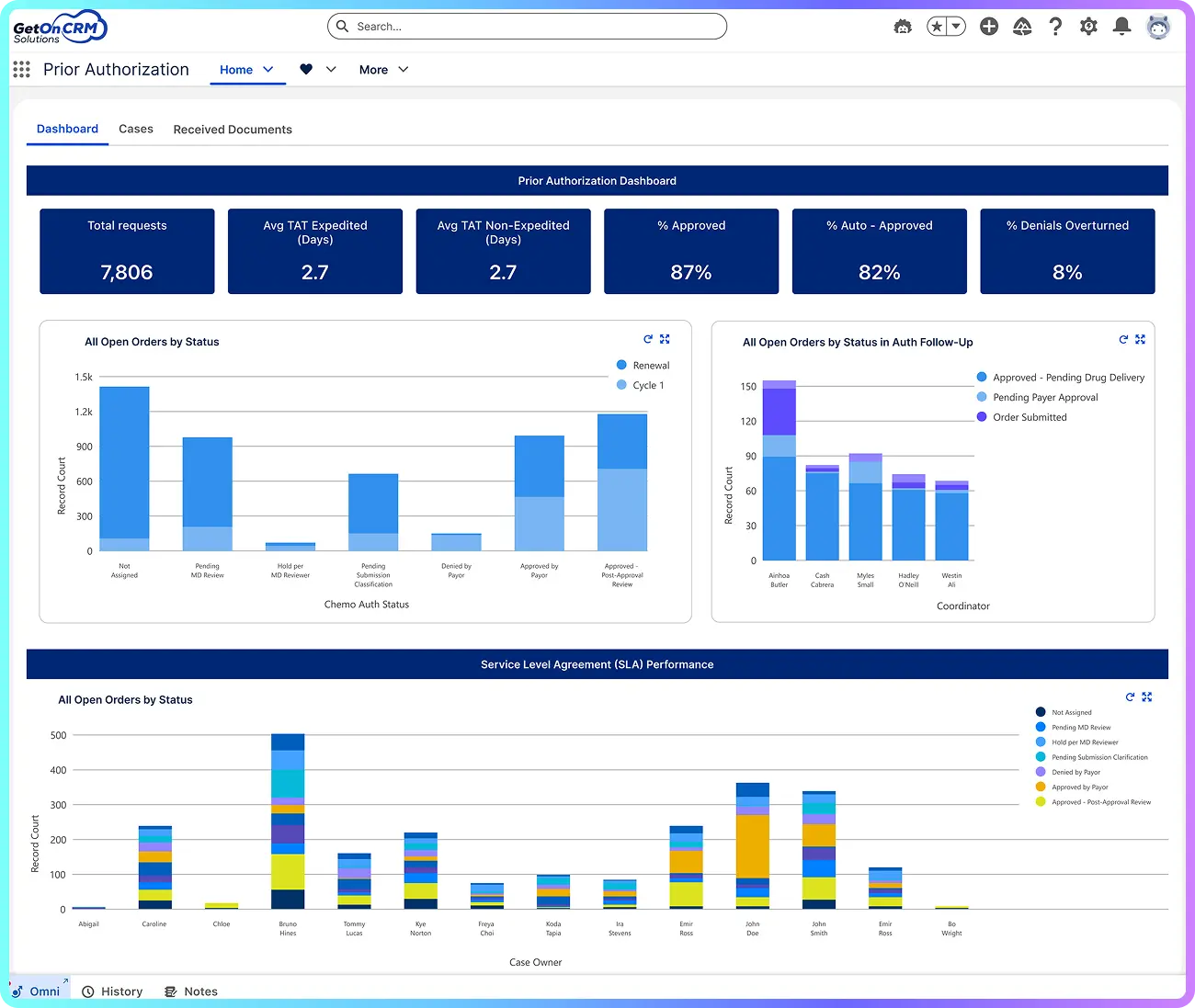
Supervisors now track real-time dashboards to view overdue cases, SLA adherence, and team performance. Every action is logged for compliance audits, ensuring the system meets healthcare governance standards.
Scalable, Secure Architecture
The platform safeguards Protected Health Information (PHI) through strict access controls. It scales easily to manage thousands of daily Prior Authorization requests without sacrificing performance or security—delivering sustainable healthcare automation using Salesforce.
Core platform for authorization management
Automated validation of payer logic
Real-time visibility and audit tracking
Real-time visibility and audit tracking
Compliant Secure Data Architecture
Compliant Secure Data Architecture
Automation logic and backend process configuration
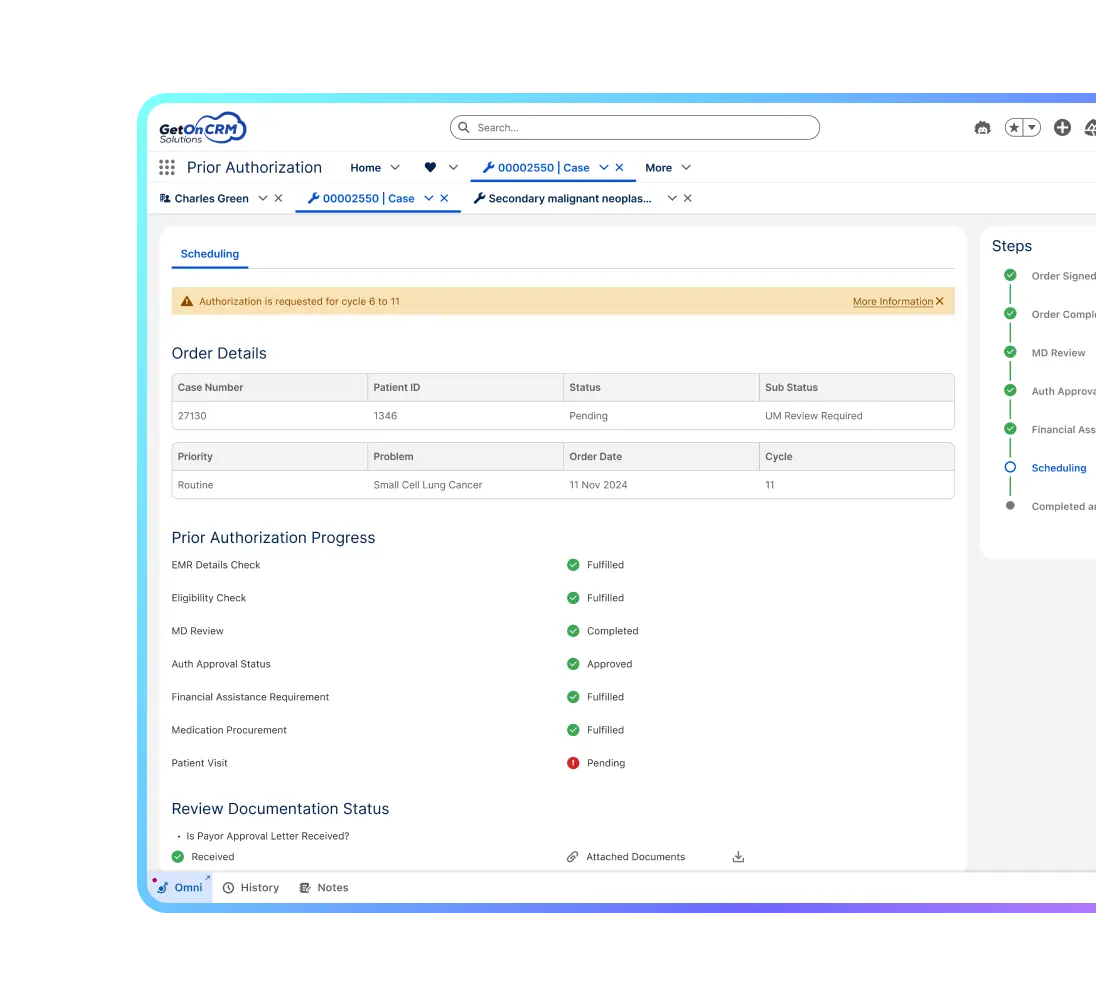
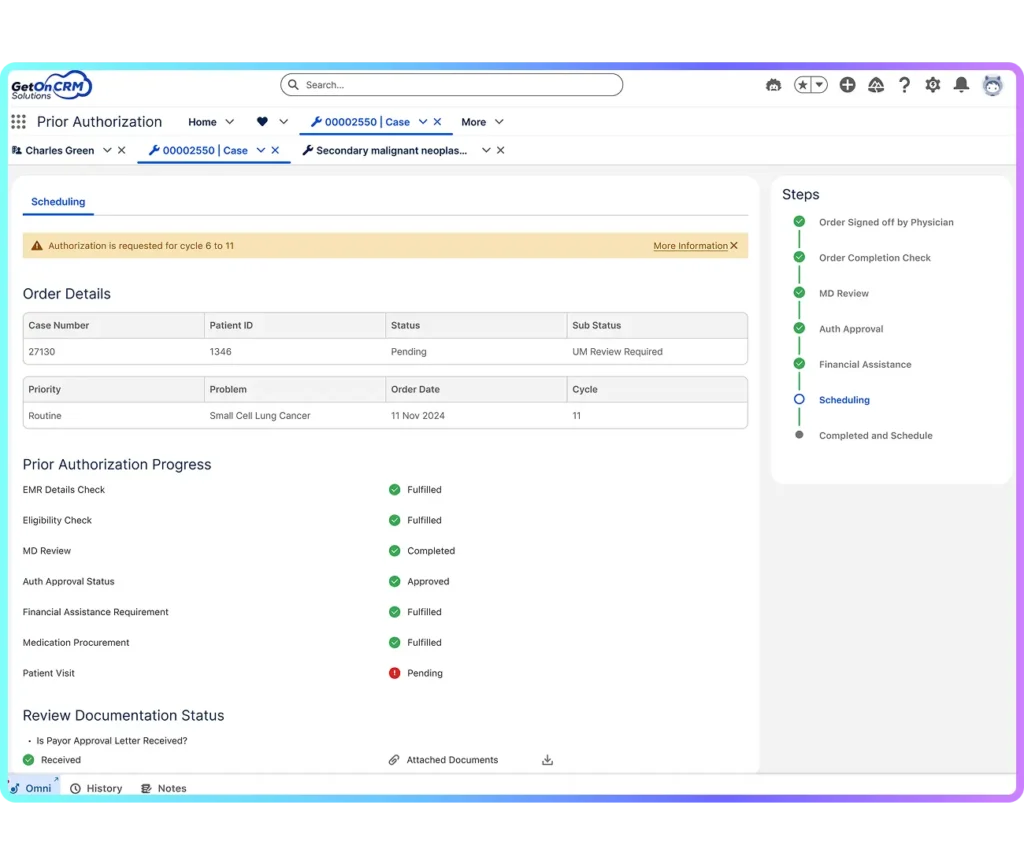
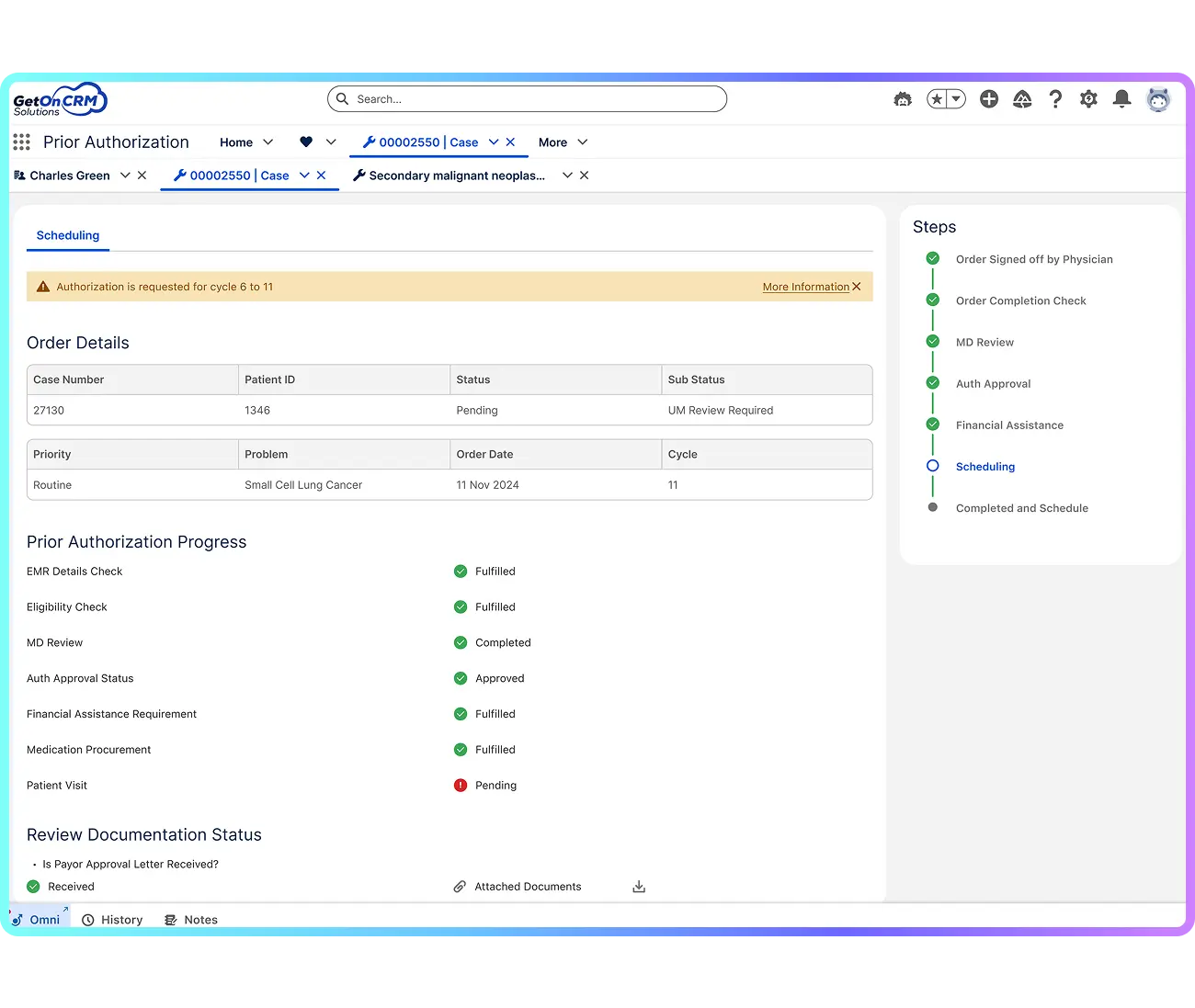
Guided workflows for structured team handoffs
Secure interoperability between EMR and Salesforce
Secure interoperability between EMR and Salesforce
We followed a structured, role-based implementation strategy to ensure seamless transition from spreadsheets to Salesforce automation.
Data Integration & Case Intake
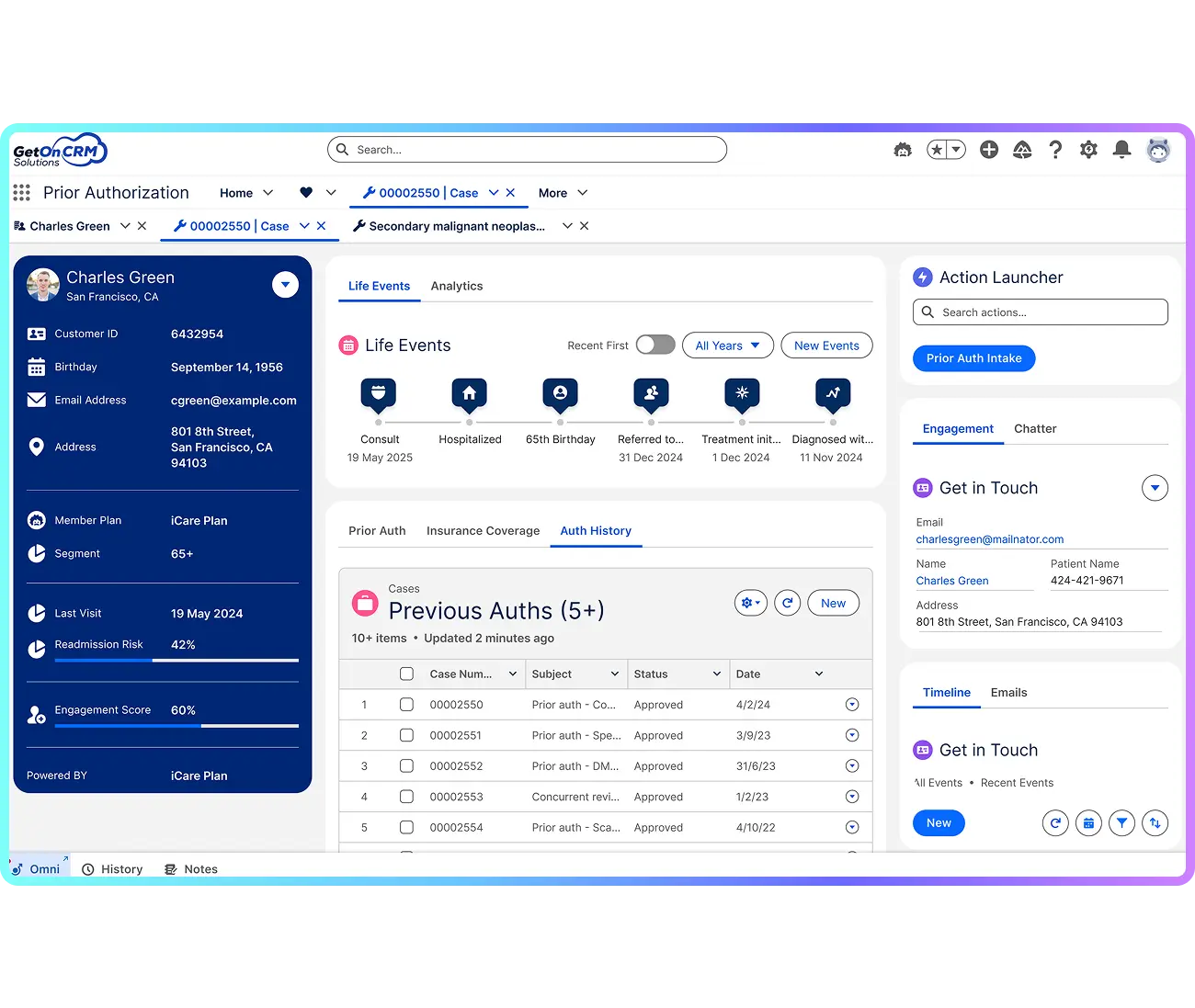
Using FHIR-based APIs, orders and patient data from the EMR flowed directly into Salesforce, auto-creating authorization cases enriched with clinical and insurance details.
Intelligent Case Routing
The Business Rules Engine automatically applied payer logic, demographics, and authorization type at intake to route cases based on treatment category—such as chemotherapy, pathology, or diagnostics—and insurance model, including Fee-for-Service or Capitation.
Role-Based Workflows
Each department operated through guided flows—submitters completed payer-required documents, coordinators managed approvals and denials, and finance validated co-pays post-approval.
Real-Time Visibility
Supervisors accessed dynamic dashboards tracking live workloads, overdue cases, and SLA compliance, ensuring accountability across teams.
Scalable & Secure Deployment
The HIPAA-compliant Salesforce architecture ensured strict role-based access control while scaling seamlessly to handle thousands of cases daily.










We are Salesforce Ridge Consulting Partner having 100% salesforce certified team.








Copyright © 2026 GetOnCRM Solutions PVT. LTD. All Rights Reserved.